
SPOTLIGHT ON ABORTION CARE & REPRODUCTIVE JUSTICE
IVF & the Legal Landscape in the United States: Part 1
Written by Sarah Osborn, AMSA Gender & Sexuality Action Committee, Reproductive Justice Coordinator
In Vitro Fertilization (IVF), an assisted reproductive technology (ART), is used to treat infertility medically and is the most common form of ART used in the United States. However, the current legal landscape greatly impacts accessibility and affordability. In the simplest terms, IVF is the process of retrieving eggs from a person’s ovaries, fertilizing them with sperm in a laboratory, and implanting that fertilized egg (embryo) into a person’s uterus with the goal of pregnancy. The first step of the IVF process begins with ovarian stimulation, also known as ovulation induction. This step involves multiple fertility medications like injectable human menopausal gonadotropin (hMG), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and human chorionic gonadotropin (hCG) to stimulate ovaries to grow multiple eggs, instead of the single egg, during a month. Generally, people will undergo 8-14 days of stimulation before eggs are retrieved. The egg retrieval is the second step and occurs before ovulation. This process is usually accomplished by transvaginal ultrasound aspiration, a minor and quick surgical procedure typically performed in an outpatient setting. After the eggs are retrieved, patients can either go straight to fertilization or store their eggs, which is called cryopreservation.
If the goal is immediate pregnancy, the eggs are combined with sperm in a laboratory. Not all eggs are used; they are examined first for maturity and quality, and those that meet standards are placed in an IVF culture medium, transferred to an incubator, and inseminated. Sometimes, motile sperm is put into the medium with the oocytes. Still, other times, intracytoplasmic sperm injection (ICSI) is needed, but both result in the same overall pregnancy and delivery rates. ICSI is a procedure in which a single sperm is directly injected into each mature egg, which is done in approximately 60% of cycles in the US. Not all mature eggs will fertilize. Usually, 65-75% make it to the culture stage, where the fertilized eggs are incubated in a laboratory to develop. However, patients can also choose to have their fertilized eggs undergo cryopreservation at this stage. If the patients want immediate pregnancy, once the embryo is ready, the patient undergoes a procedure to implant the embryo into the uterus, which typically occurs in the physician’s office. Usually, multiple embryos are implanted, and the maximum number of implanted embryos is based on calculations from patient and embryo characteristics.
Cryopreservation can occur at multiple points during IVF, leading to either eggs or embryos being frozen for future use. There are two methods for cryopreservation. One is the conventional “slow” freezing, and the other is vitrification “fast” freezing. Cryopreservation can simplify future ART cycles by cutting costs due to not needing to repeat the IVF cycle, which includes medications and egg retrieval, and allowing it to start at the fertilization or transfer stage. The frozen eggs and embryos can be stored for long periods, with live births recorded from a 20-year-old frozen embryo. While freezing eggs/embryos is a great way to help provide future family planning, not all eggs/embryos will survive the freezing and thawing process. It is also essential to consider at which stage to freeze since eggs are only from one person, while embryos are from two people, leading to more potential legal issues (discussed in part 2).
The IVF process can be long, daunting, and costly, and the current legal landscape makes it a difficult battle. However, this process has been around for more than 30 years and provides people with options for family planning. In the US, since, an estimated 1 in 8 women of reproductive age have received infertility services, which includes IVF. In 2021, 453 US fertility clinics provided 413,776 ART cycles to 238,126 patients. These cycles resulted in 97,128 live-born infants, representing 2.3% of all infants born in the US that year. However, not all of those ART cycles had the intent to transfer an embryo; 41% (167,689 out of 413,776) of those cycles had the purpose of storing the eggs/embryos via cryopreservation for potential future use. When looking at all age groups of patients going through ART cycles, around 80% of transplantation procedures used frozen embryos instead of an immediate transfer.
The use of ART has grown throughout the years, and people have used it for many reasons. The most common cause is infertility, for example, females experiencing endometriosis or males with low sperm count. Other reasons to pursue IVF include preserving future fertility for patients who are dealing with chronic illnesses like lupus or patients who want to have children in the future but are not ready yet. Patients diagnosed with cancer also seek fertility preservation before they start chemotherapy/radiation, and this has become considered a standard of care.
Even though many people in the US are using IVF, and it is leading to people having options for family planning, the procedures can be costly, especially since multiple cycles are often needed to have a successful conception. One estimation of a single cycle of IVF was between $15,000-$20,000 but can exceed $30,000. The average number of cycles needed for successful conception is 2.5, so the average IVF cost easily exceeds $40,000. A California clinic reported that their average out-of-pocket cost for a successful outcome was $61,000. That is a huge bill to pay, and since IVF treatment is usually not covered by insurance, it has created a socioeconomic divide in who can go through IVF. Every state has different requirements for IVF coverage, including Medicaid coverage, private insurance, and self-insured plans.
Insurance can be complicated, and with state laws varying on coverage for infertility services, it can make it difficult for people to get insurance coverage for IVF. Of note, companies/employers that “self-insure” do not have to follow state insurance regulations because they are exempt due to “The Employment Retirement Income and Security Act of 1974”. The first thing to consider is if there is a coverage mandate. This is a state law consisting of a “mandate” of what insurance has to offer/cover in terms of infertility treatment. These mandates will include what type of insurers are required to follow the mandate, if there is a cap on how much coverage must be provided, eligibility requirements (i.e. age restrictions, number of IVF cycles covered, waiting period), limitations (i.e. how does the law define infertility, does it apply to only opposite sex married couples or does it include single people and same sex couples), and what exemptions can be made.
State IVF Coverage Mandates
(Successful pregnancy is defined as a pregnancy ending in a live birth)
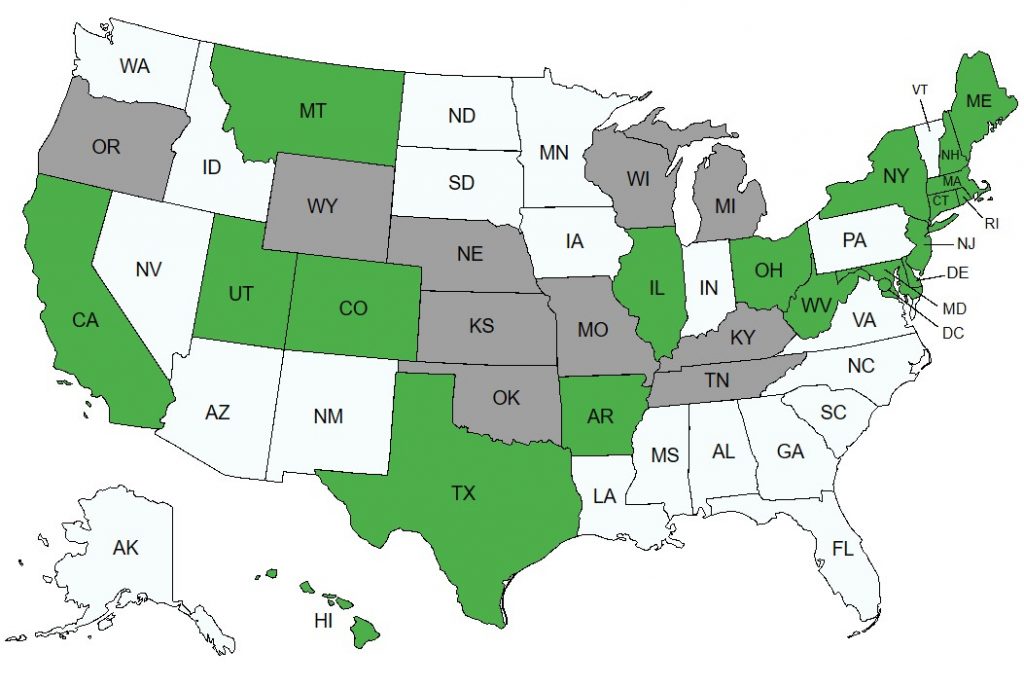
Map Key:
Green = States with IVF Coverage Mandates
Grey = States with IVF Exclusions or Limiting Laws
White = States without IVF Coverage Mandates
Find Details on State IVF Coverage Mandates – Here
States Fertility Preservation Coverage Mandates
(which is storing eggs/sperm/embryos for later use such as cryopreservation from an IVF cycle)
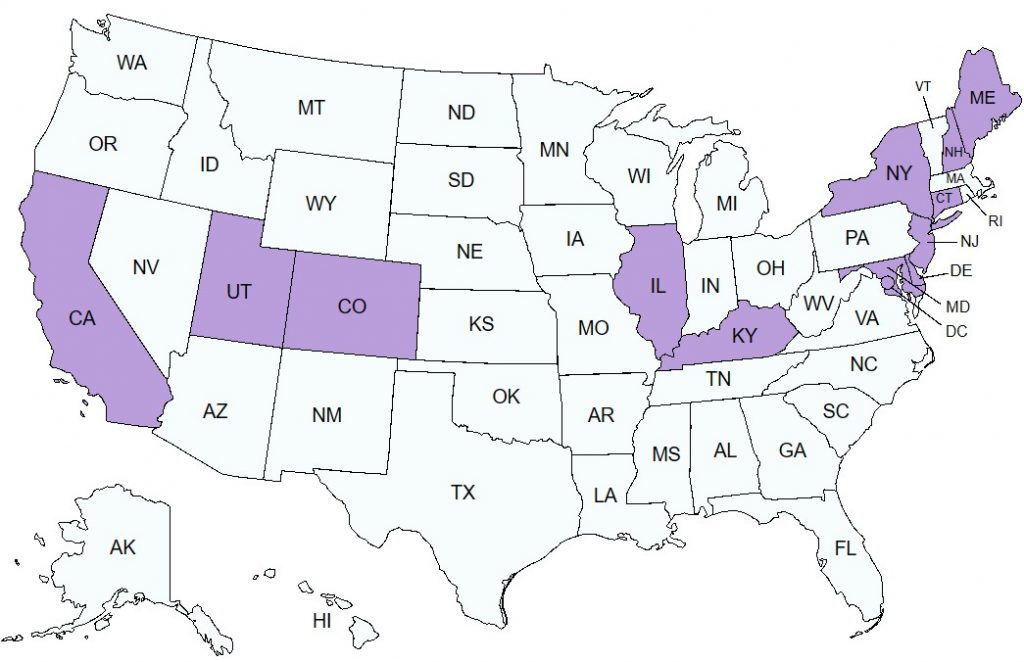
Map Key:
Purple = States with Fertility Preservation Coverage Mandates
White = States without Fertility Preservation Coverage Mandates
Find Details on States Fertility Preservation Coverage Mandates – Here
Not only do insurance laws complicate IVF options and make it difficult for those seeking IVF to get coverage, but state laws affecting reproductive rights also affect IVF. Be on the lookout for part 2, which will include the current laws and legal considerations for egg/embryo storage and unused eggs/embryos. Part 2 will also include how the laws affect patients and how it affects you as a future physician.
Resources and more information about IVF
- American Society for Reproductive Medicine (ASRM): https://www.asrm.org/
- ReproductiveFacts.org
- More details about state insurance laws: https://www.reproductivefacts.org/patient-advocacy/state-and-territory-infertility-insurance-laws/
- 6 Fact sheets pertaining to IVF: learn more about the process of IVF and the risk factors, and questions to ask potential clinics: https://www.reproductivefacts.org/news-and-publications/fact-sheets-and-infographics/?q=IVF&s=title&r=SearchCategories[TOPICS%7eIn+Vitro+Fertilization+(IVF)]
- CDC ART: https://www.cdc.gov/art/
- SART (Society for assisted reproductive technology) : https://www.sart.org/#
- NIH State Pearls: https://www.ncbi.nlm.nih.gov/books/NBK562266/
- U.S. Department of Health and Human Services: https://www.hhs.gov/about/news/2024/03/13/fact-sheet-in-vitro-fertilization-ivf-use-across-united-states.html#:~:text=IVF%20represents%20greater%20than%2099,%2C%20Pennsylvania%2C%20Virginia%20and%20Georgia.
###
*Note: an excerpt of this Spotlight is included in AMSA Reproductive Health Project eNews
#38 Shield Laws Protect Providers & Increasing Attacks on Abortion Rx – Feb 15, 2025
Find the current and past issues in the AMSA Repro eNews Archive.
