SPOTLIGHT ON HEALTH & REPRODUCTIVE JUSTICE
You Shouldn’t Have to See a Bill Before You See Me
The Affordable Care Act Now and in the Future
Written by an AMSA student member who requested anonymity
in light of recent disappearances of students by the Trump Administration’s ICE & CBP
The number of days left in my medical school career is quickly coming to an end. I can’t say I have seen or learned everything I need to know, but these past four years have laid a solid medical foundation for the next stage in my life.
What I still feel unsure about is my understanding of the cost and
financial structure upholding medical care in the US.
What knowledge I have has been pieced together from my personal experience working in the field, short segments within lectures and exchanges I have observed between physicians and their patients or staff. I rarely receive a good answer when I express my concern about the lack of education in how the financial infrastructure of the medical industry runs.
Starting residency training in this way feels like navigating a maze with only half of the map.
During my elective rotations, I witnessed a painful appointment where a patient had experienced a second trimester loss. She sat with her husband trying to maintain her composure but the further she went into the conversation with the attending physician, the more distressed she became; understandably so. This was the first of two appointments for a dilation and evacuation (D&E). The atmosphere was extremely somber, her grief was palpable, and extended into her appointment for the procedure itself.
Before the end of the procedure, the patient lifted her head up still in lithotomy position
to ask for a total price estimate of the care she was receiving.
She did this because her insurance had been emphatic about the fact that they would not cover a D&E procedure. The atmosphere in the room shifted from being solemn to tight and uncomfortable. Every caretaker in the room tensed imperceptibly. The question was of course routed to the financial assistance team with assurance of a payment plan option if necessary but the discomfort never truly dissipated after that.
The unfortunate truth that is always sitting in the room with every patient and provider made itself known.
The cost of health care in America is very expensive.
Before The Patient Protection and Affordable Care Act (ACA) was signed into law in 2010, 14-16% of US citizens across all ages were uninsured. The ramifications of this cannot be overstated. In the intervening 15 years over 44 million people have gained coverage through the ACA: 21.3 million through ACA marketplaces and an additional 21.4 million people through ACA supported expansion of Medicaid across 41 states and D.C. This law aimed not only to expand coverage across the population, but to also establish health insurance regulations designed to protect all individuals with both private and public coverage from industry-wide discriminatory practices like automatic denials, higher premiums, or coverage exclusions due to pre-existing conditions. The ACA is far from perfect but it was established with a common understanding that every individual no matter their income or health status should be able to access affordable health care coverage.
The harms of no insurance coverage and exploitative insurance policies affect
not just the patient but the medical caregivers as well.
Among the flood of executive orders, agency defundings and the aggressive attempt to establish a new understanding of America’s values, the president has demonstrated that his ‘concepts of a plan’ to improve upon the current health finance infrastructure is to cripple it at the knees for the most vulnerable, often hiding behind the objective of curbing government spending. This has taken the form of changing insurance payment formulas, eliminating the Low-Income Special Enrollment Period (SEP), and changing the definition of ‘law presence’ so that it excludes DACA recipients to mention a few. The inevitable consequences of these changes include an increase in premium and out-of-pocket costs and a lower threshold for insurance companies to refuse coverage for vulnerable individuals. Watching providers navigate insurance stipulations and observing how these policies shape how medicine is practiced, when a certain treatment can be administered, and the puzzling need to provide financial justification for a life-saving therapy, already seemed difficult and frustrating enough.
The changes now underway by the Administration and under consideration by Congress
make the looming figure of cost even larger in the patient-physician relationship.
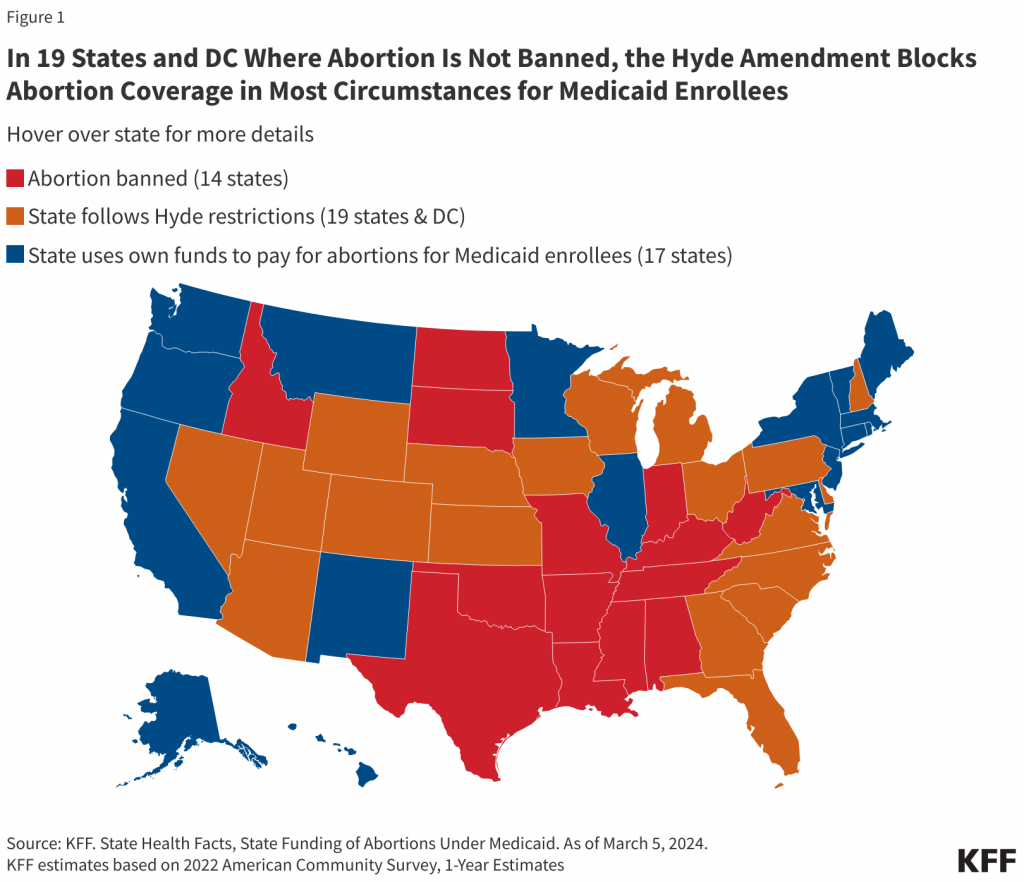
Although the Hyde Amendment prohibits spending of federal tax dollars on abortion care, a s of 2024, 17 states allow Medicaid coverage of abortion care through state funds.
The cost of abortion care without health coverage becomes an increasing burden and barrier to care the further along in gestation a patient is. The cost leaps between the medical and surgical management of these cases.
Being in the room with that patient after she had asked for a price estimate made me feel irrevocably sad.
My sadness was intertwined with helplessness and anger.
I understand that providing medical care comes at a cost. I understand that in our current “system” costs will be shared between the government, insurance companies and patients in the best scenario. But I don’t understand how a government that includes people with health concerns, chronic illnesses, pregnant family members, and members grieving from devastating diagnoses themselves refuse to lean into the very visceral and physical experience of the human condition and commit to make it safer and affordable for people both at their best and worst.
Becoming a doctor in the U.S. at a time when I feel such dissonance with the medical institution, the government and executors of what I can or cannot provide patients in the form of insurance companies feels like walking into that same maze, with half of the map, and little light to guide me forward.
I decided to look up the cost of dilation and evacuation procedures and learned that it can reach as high as $10,000 in the hospital outpatient setting.
Ten Thousand Dollars
The fact the patient is going to have to endure the emotional, physical and financial burden of a devastating outcome and had to peripheralize the grief and pain she was in to ‘get the check’ before leaving is unacceptable. The Affordable Care Act was a step away from this, and a step toward joining the rest of the so-called first world in guaranteeing affordable, accessible health care for all. Now 15 years later, the hard-won protections and expansions that were put in place are in grave danger of being stripped away.
Practicing medicine is already hard enough. Being a patient is certainly harder.
It is my responsibility to be prudent and thoughtful about the resources that I use in the process of caring for my future patients but it should not be a burden or barrier to the care that patients can access.
The ideal and philosophy that my training has rested on thus far is that
the patient-physician relationship is just that: a relationship.
It shouldn’t feel transactional, dehumanizing or isolating.
In the room with that patient, all three of these threatened to break down the trust and supportive care she was being provided at that moment.
My hope is that the more I learn and understand the financial infrastructure of American healthcare, the more I can be involved in ways to support patients in navigating it, and ultimately in addressing the root causes themselves, the closer we will be to a just and fair health care system in the U.S. that guarantees high-quality, affordable, accessible for all.
When a patient walks into the clinic or hospital, the only thing I want them thinking about is how to reach their goals of wellness and health; not the bill.
###
Learn more about ACA protections, benefits here:
Reproductive Justice & 15 Years of The Affordable Care Act
*Note: an excerpt of this Spotlight is included in AMSA Reproductive Health Project eNews
#43 Frontline Voices & Summer Essay Contests – Win Cash, Get Published! – April 12 2025
Find the current and past issues in the AMSA Repro eNews Archive.
Explore the AMSA Reproductive Health Project
Find news, tips, tools, opportunities & more!
Sign-up Here for AMSA Repro Project Updates