IVF & Fertility Preservation Across the United States
Scroll Down To Learn More About Your State
Learn More in AMSA On Call
SPOTLIGHT ON ABORTION CARE & REPRODUCTIVE JUSTICE
IVF & the Legal Landscape in the United States: Part 1
Written by Sarah Osborn, AMSA Gender & Sexuality Action Committee, Reproductive Justice Coordinator
State IVF Coverage Mandates
(Successful pregnancy is defined as a pregnancy ending in a live birth)
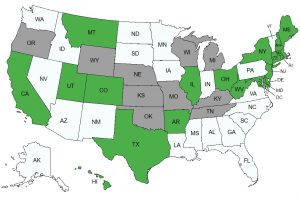
Map Key:
Green = States with IVF Coverage Mandates
Grey = States with IVF Exclusions or Limiting Laws
White = States without IVF Coverage Mandates
Arkansas (Effective 9/2/1991)
-
- Coverage Mandate: All accident and health insurance companies that have any business in the state must include IVF as a covered expense. IVF is not defined, but the law states the cryopreservation is included as an IVF procedure.
- Scope of Mandate: Rule applies to insurance policies for individuals, groups, or blankets that were issued/renewed in the state, or those delivered in the state. Also includes disability insurance of any state resident, even if their group policy is from outside the state, as long as the policy provides normal pregnancy-related benefits. (Guidance suggests that the policy does not apply to HMOs, but no clear language is set)
- Coverage Cap: Lifetime maximum benefit of $15,000
- Requirements/Limitations: IVF benefits must be the same as maternity benefits (this means that patients undergoing IVF may have the same deductibles, co-insurance, and out-of-pocket pay as stated in maternity benefits), and must meet all the following criteria:
- Patient must have failed to have a successful pregnancy from other less costly infertility treatments covered by their insurance
- Patient’s oocytes must be fertilized with spouse’s sperm
- Patient and spouse must have at least 2 years of unexplained infertility (or documentation of infertility caused by endometriosis, exposure to DES in utero, dysfunction or one or both fallopian tubes (excluding voluntary sterilization), or abnormal male factors)
- IVF performed at state licensed medical facility that follows ACOG or ASRMs guidelines for IVF
- Exemptions: Minimum basic benefit policies and Comprehensive Health Insurance Pool policies are prohibited from covering IVF
California (Effective 1/1/1990)
-
- Coverage Mandate:Insurers must offer infertility treatment coverage, but are not required to cover IVF. In 2022, an amendment to the mandate was made (AB-797) which changed the bill language to include infertility to LGBTQ+ and single people.
- Mandate’s definition of infertility: patient must provide a condition documented by a physician as the cause of their infertility or have been unable to have a successful pregnancy after at least a year of unprotected sexual intercourse
- Scope of Mandate: Any insurers and HMOs with at least 20 employees. The 2022 amendment also requires commercial insurers to cover infertility treatment.
- Requirements/Limitations: Insurers are not required to cover treatment, however, they must offer services to employers who then decide if they will provide infertility benefits to their employees.
- Exemptions: Insurers are only required to offer infertility treatment and they do not have to cover chosen treatment. Do not have to offer IVF treatment. Religious organizations do not have to offer coverage.
- Coverage Mandate:Insurers must offer infertility treatment coverage, but are not required to cover IVF. In 2022, an amendment to the mandate was made (AB-797) which changed the bill language to include infertility to LGBTQ+ and single people.
Colorado
-
- Coverage Mandate: Any insurance plan issued or renewed in Colorado must cover diagnosis and treatment of infertility.
- Mandate’s definition of infertility: any disease or condition that causes the inability to reproduce. This can be as an individual, or as a couple.
- Mandate’s definition of diagnosis and treatment of infertility: any procedures/medications recommended by Colorado licensed physicians that are congruent with approved practices or professional guidelines from ACOG or ASRM.
- In 2023, an update to the mandate now includes that health plans covering more than 100 employees must cover the diagnosis and treatment for infertility which follows ASRM guidelines to include 3 complete oocyte retrievals with unlimited embryo transfers.
- Scope of Mandate: Any health plans provided to individuals or groups in the state.
- Requirements/Limitations: Plans may not impose exclusion, limitations, or restrictions on coverage for fertility medications or any copayments, coinsurance, benefit maximums, waiting periods, or other limitations for fertility coverage (diagnosis, treatment, or preservation services). Any fertility service may only have the same limitations set by the health benefit plan for any medications or services.
- Exemptions: Religious employers can request an exemption.
- Coverage Mandate: Any insurance plan issued or renewed in Colorado must cover diagnosis and treatment of infertility.
Connecticut
-
- Coverage Mandate: Insurance policies (individual and group) must provide coverage for diagnosis and treatment of infertility. Has language to directly include IVF treatment.
- Mandate’s definition of infertility: any individual who cannot produce a successful pregnancy during a one-year period.
- Scope of Mandate: Medicaid programs do not cover infertility diagnosis or treatment.
- Coverage cap: Based on fertility treatment
- Lifetime maximum coverages: 4 cycles of ovulation induction, 3 cycles of intrauterine insemination, 2 cycles of IVF/GIFT/ZIFT/or low tubal ovum transfer.
- In order to gain coverage for IVF, GIFT, ZIFT, and low tubal ovum transfer, must first try less expensive infertility treatments covered by insurance.
- Infertility treatments and procedures must be in clinics that abide by guidelines from ASRM and the Society of Reproductive Endocrinology and Infertility.
- Requirements/Limitations: Patients must provide proof that treatment is medically necessary or are not able to produce a successful pregnancy during a one-year period.
- Exemptions: A religious employer (defined as a qualified church-controlled organization) can submit a written request to exclude fertility coverage.
- Coverage Mandate: Insurance policies (individual and group) must provide coverage for diagnosis and treatment of infertility. Has language to directly include IVF treatment.
District of Columbia
-
- Coverage Mandate (started January 1st, 2024): The DC Healthcare Alliance program provides health insurance coverage for diagnosis and treatment of infertility. Includes at least 3 cycles of ovulation-enhancing medication.
- Currently fertility coverage amendments are being made to the Medicaid state plan.
- Coverage Mandate beginning January 1st, 2025: All insurers that offer any health benefit plans (including individual, small or large group plans) are required to provide coverage for diagnosis and treatment of infertility and fertility preservation services. Direct language includes:
- Three rounds of IVF
- For patients with oocyte retrievals performed prior to January 1st, 2025, they must be covered for unlimited embryo transfers from prior oocyte retrievals and given the opportunity for at least 3 new complete oocyte retrievals
- Must cover any medical costs from an embryo transfer from an covered individual to a third-party (the covered costs do not extend after the embryo transfer procedure, i.e. will not cover medical costs of the surrogate)
- Coverage Mandate (started January 1st, 2024): The DC Healthcare Alliance program provides health insurance coverage for diagnosis and treatment of infertility. Includes at least 3 cycles of ovulation-enhancing medication.
Delaware (Effective 6/30/2018)
-
- Coverage Mandate: Any insurance policies must cover fertility care services for patients with infertility. Includes IVF treatment. Benefits cover individuals (and their covered spouses and dependents) and must provide coverage of the same extent as all other pregnancy-related services. Policies cannot impose any limitations or extra costs that are different from their other services not related to fertility.
- Mandate’s definition of infertility: any disease or condition that causes impaired reproduction in which an individual cannot procreate or carry a pregnancy to live birth.
- Scope of Mandate: Includes all insurance plans, policies, contracts, or certificates for individuals, groups, or blanket coverage. Direct language includes HMOs.
- Requirements/Limitations: To qualify for coverage, all the following must be met:
- Patients must have a physician’s diagnosis of infertility, or documented risk of iatrogenic infertility. (Physician must be a obstetrician-gynecologist, reproductive endocrinologist, oncologist, urologist, or andrologist)
- Patients have tried covered less costly infertility treatments without successful pregnancy.
- if IVF is medically necessary policy cannot require ovulation induction or intrauterine inseminations before IVF is covered
- Patients are not required to go through more than 3 cycles of ovulation induction or intrauterine inseminations before IVF is covered
- IVF procedures must be done in clinics that follow guidelines by ASRM and ACOG
- IVF retrievals must be completed before the patient is 45 years old, and transfers before the patient is 50 years old
- Exemptions: For a group or blanket policies from religious organizations, they may request (and must be granted) exclusion from coverage fertility treatments. Small businesses with less than 50 employees are automatically exempt.
- Coverage Mandate: Any insurance policies must cover fertility care services for patients with infertility. Includes IVF treatment. Benefits cover individuals (and their covered spouses and dependents) and must provide coverage of the same extent as all other pregnancy-related services. Policies cannot impose any limitations or extra costs that are different from their other services not related to fertility.
Hawaii (Effective 6/26/1987)
-
- Coverage Mandate: Any plan that covers pregnancy-related benefits must cover infertility treatments and cover all outpatients expenses from 1 IVF cycle.
- Scope of Mandate: Applies to individual and group insurance policies including hospital, medical service plan contracts, accident, health, or sickness policies, that provide any pregnancy-related benefits.
- Requirements/Limitations: All requirements must be met to qualify for 1 covered IVF cycle
- The benefit given is to the same extent as the policies other pregnancy-related benefits
- The patient is the directly covered by the health plan, or is the dependent of someone covered by the health plan
- The patient’s oocytes are fertilized with their spouse’s sperm (spouse defined as lawfully married under state laws)
- The patient and spouse have 5 years of infertility or infertility due to a medical condition (endometriosis, exposure to DES in utero, dysfunction/removal of fallopian tube, abnormal male factors)
- Patient has failed to have a successful pregnancy through other covered treatments
- IVF is performed at a clinic that follows guidelines from ACOG or ASRM
Illinois
-
- Coverage Mandate: Insurers that provide pregnancy related benefits must provide infertility treatments. Direct language includes infertility diagnosis, IVF, GIFT, ZIFT, low tubal ovum transfer, uterine embryo lavage, embryo transfer, and artificial insemination.
- Scope of Mandate: Only mandates that group insurers with more than 25 employees and HMOs that offer pregnancy benefits provide infertility treatments.
- Coverage cap: Up to four egg retrievals. However, if a patient has a live birth, coverage will be provided for an additional two egg retrievals (lifetime maximum of six)
- Requirements/Limitations
- For patients to be covered for IVF, GIFT, and ZIFT they must first go through less costly covered treatments without successful pregnancy
- Procedures must be done at clinics that follow ACOG and ASRM guidelines
- Exemptions: Religious employers and employers with less than 25 employees are exempt.
Maine (Effective January 1st, 2024)
-
- Coverage Mandate: Any health plan must provide coverage for fertility diagnostics and if the patient is deemed a “fertility patient” then fertility treatment must be covered.
Maryland (Effective 10/1/1997)
-
- Coverage Mandate: All plans that provide pregnancy-related benefits cannot exclude benefits for any expenses from outpatient IVF procedures. Covers the policyholder and their dependent spouse. Plans do not have to cover any costs for obtaining donor sperm.
- Coverage Scope: Any insurers and nonprofit health plans must provide the same extent of benefits for other pregnancy-related procedures. HMOs must provide the same extent of benefits for any other infertility service.
- Coverage Cap: Insurers, plans, or HMOs may limit coverage to a maximum of 3 IVF attempts per live birth. Maximum lifetime benefit is set at $100,000.
- Requirements/Limitations:
- All requirements must be met to qualify for coverage
- Patient is the policyholder or dependent
- Patient tried less costly covered infertility treatment without successful pregnancy
- IVF procedures are performed at clinics that follow medical guidelines
- For married patients with a spouse of the opposite sex the patient’s oocyte must be fertilized with spouse’s sperm (exceptions for abnormal male factors resulting in viable sperm, not from voluntary sterilization)
- For married patients the patient and spouse must have a involuntary infertility history or have at least one of the following conditions: endometriosis, in utero exposure to DES, dysfunction/removal of one/both fallopian tubes, or abnormal males factors
- If a patient and spouse are of opposite sex, involuntary infertility is defined as no successful pregnancies with at least 1 year of intercourse
- If a patient and spouse are of the same sex, involuntary infertility is defined as no successful pregnancies with 3 attempts of artificial insemination in 1 year.
- For unmarried patients they either must have infertility associated with endometriosis, in utero exposure to DES, dysfunction/removal of one/both fallopian tubes, or in the past year has not had a successful pregnancy from 3 attempts of artificial insemination
- All requirements must be met to qualify for coverage
- Exemptions: Religious organizations may request exemption which must be granted by the insurer, nonprofit health service plan, or HMO. Small business employers are automatically exempt.
Massachusetts
-
- Coverage Mandate: All policies providing pregnancy-related benefits must provide their policyholders the same coverage medical expenses necessary for the diagnosis and treatment of infertility. Infertility is defined as the inability to conceive/produce conception, or have a live birth pregnancy in a certain time frame. 1 year period if female is less than 35, 6 month period if female is over 35.
- Coverage Scope: Only applies to policies that already cover pregnancy-related benefits including general policies in or out of the commonwealth, accident/sick policies in the commonwealth, state issued employee health and welfare funds, subscription certificates, individual/group hospital service plans, and HMOs.
- Exemptions: Any supplemental policies for Medicare or other government insurance are automatically exempt.
Montana (Effective 1987)
-
- Coverage Mandate: HMOs must provide infertility services in covered basic health care services, however, coverage law does not define which services are included.
- Scope of Mandate: Only HMOs.
New Hampshire (Effective 1/1/2020)
-
- Coverage Mandate: Health carriers must cover any medically necessary fertility diagnosis and treatment. Direct language includes treatments that utilize donor eggs, sperm, and embryos. Infertility is defined as a disease causing the inability to become pregnant or to carry pregnancy to live birth or the partner’s inability to cause pregnancy.
- Scope of Mandate: Applies to all health carriers, which is any entity that follows insurance laws or provides/interacts with any costs of healthcare services. Direct language includes insurance companies and HMOs.
- Requirements/Limitations: Health carriers cannot impose any limitations, maximum benefits, extra charges, or pre-existing condition exclusions that are different from any other service or medication they cover not related to infertility.
- Exclusions: Mandate does not apply to any health coverage through the Small Business Health Options Program or to Affordable Care Act-Compliant Policies.
New Jersey (Effective 11/29/2001)
-
- Coverage Mandate: Any insurers that provide any medical or hospital benefits must cover any medically necessary expenses from diagnosis and treatment of infertility. Direct language includes IVF, IVF using donor eggs, and IVF using a gestational carrier or surrogate.
- Mandate’s definition of infertility: any disease or condition that alters the function of the reproductive system determined by a Reproductive Endocrinology and Infertility or in Obstetrics and Gynecology physician following ASRM guidelines. Or, if the patient meets at least one of the following conditions:
- A male who is unable to impregnate a female
- A female with a male partner unable to to conceive after a set time based on age of unprotected sexual intercourse (12 months if under 35 years of age, 6 months if over 35 years of age)
- A female without a male partner unable to conceive after a set number of failed medical intrauterine insemination attempts based on age (12 failed attempts if under 35 years of age, 6 failed attempts if over 35 years of age)
- Partners unable to conceive due to iatrogenic infertility
- A person who is unable to carry a pregnancy to live birth
- Mandate’s definition of infertility: any disease or condition that alters the function of the reproductive system determined by a Reproductive Endocrinology and Infertility or in Obstetrics and Gynecology physician following ASRM guidelines. Or, if the patient meets at least one of the following conditions:
- Scope of Mandate: Applies to any health based insurers including health service corporations, hospital service corporations, medical service corporations, and health insurance companies.
- Coverage Cap:
- Maximum of 4 complete egg retrievals during that person’s lifetime
- Requirements/Limitations:
- Infertility due to voluntary sterilization is excluded
- Patients must be less than 46 years of age
- Patient has attempted pregnancy through less expensive covered infertility treatments without any successful pregnancy
- Cryopreservation is not covered unless the patient needs medical treatment that can result in iatrogenic infertility
- Coverage does not include sperm or oocyte storage
- Exemptions: Any small employers defined as having less than 50 employees. Any religious employer is not required to cover the mandate. Mandate does not apply to any state funded medical assistance (i.e. Medicaid)
- Coverage Mandate: Any insurers that provide any medical or hospital benefits must cover any medically necessary expenses from diagnosis and treatment of infertility. Direct language includes IVF, IVF using donor eggs, and IVF using a gestational carrier or surrogate.
New York (Effective 1/1/2020)
-
- Coverage Mandate and Scope: Two different mandates depending on type of insurance policy.
- For large insurance policies that provide major/comprehensive medical coverage (i.e. insurance by hospital service corporations, health service corporations, large group insurance policies) must also cover 3 cycles of IVF for infertility treatment.
- Mandate’s definition of a IVF cycle: medications for ovarian stimulation and oocyte retrieval ending with intent of IVF with fresh embryo transfer or medications for endometrial preparation with the intent of IVF with a frozen embryo
- For individual or small group insurance policies , or student insurance policies must cover infertility treatment (but mandate does not specifically state what infertility treatment must cover).
- Mandate’s definition of infertility: individual is unable to have a clinical pregnancy after a set time of unprotected sexual intercourse or donor insemination (12 months for a female under 35 and 6 months for a female over 35 years of age)
- For large insurance policies that provide major/comprehensive medical coverage (i.e. insurance by hospital service corporations, health service corporations, large group insurance policies) must also cover 3 cycles of IVF for infertility treatment.
- Requirements/Limitations:
- Insurance policies cannot exclude coverage for diagnosis and treatment of medical conditions just because the treatment could result in infertility
- Coverage Mandate and Scope: Two different mandates depending on type of insurance policy.
Ohio (Effective 4/11/2021)
-
- Coverage Mandate: Insurance that covers “basic health care services” must cover infertility services. However, they do not define infertility, or which services are covered.
- Scope of Mandate: Any health insuring corporations
- Exceptions: MEWAs and Medicaid.
Rhode Island (Effective 6/16/1991)
-
- Coverage Mandate: Insurers and HMOs that cover pregnancy benefits must also cover diagnosis and treatment of infertility.
- Mandate’s definition of infertility: a presumably healthy person who is not able to conceive or carry a pregnancy after trying for one year.
- Scope of Mandate: Any health insurance that covers or provides pregnancy-related benefits. Language directly includes blanket/group policies, any nonprofit hospital/medical service contract/plan/insurance policy, any HMO service contract plan/policy.
- Coverage Cap: No direct language, but policies may set a limit of a lifetime cap of $100,000 for infertility treatments.
- Requirements/Limitations: Women seeking diagnosis and treatment must be between 25 and 42 years of age.
- Exemptions: Any insurance plan that is supplemental coverage to Medicare or other government programs.
- Coverage Mandate: Insurers and HMOs that cover pregnancy benefits must also cover diagnosis and treatment of infertility.
Texas (Effective 4/1/2005)
-
- Coverage Mandate: Any group health plan that provides or covers pregnancy-related benefits must offer coverage for IVF procedures.
- Scope of Mandate: Applies to group health insurance policies/plans/service contracts provided by any insurer, group hospital service corporation, HMO, employer, union, association, or self-insured benefit program.
- Requirements/Limitations: To qualify for any coverage, must meet all the following requirements
- Patient wanting IVF must be covered under the group health plan
- Patient’s oocytes must be fertilized only with sperm from patient’s spouse
- Patient and their spouse must have had infertility for at least 5 consecutive years or been diagnosed with endometriosis, in utero exposure to DES, dysfunction/removal of fallopian tubes, or oligospermia
- Patient has tried less costly covered infertility treatments and was unsuccessful to attain pregnancy
- IVF performed in a medical clinic that utilizes minimal standard programs for IVF.
- Exemptions: Health benefit plans through a health group cooperative do not have to offer to cover IVF. Any health plan from a religious organization (owned or part of a group) is not required to offer IVF coverage.
Utah (Effective 7/1/2020)
-
- Coverage Mandate and Scope: Applies only to Public Health Employees’ Health Plan, and those on Medicaid if they get an approved waiver. Patients with a physician diagnosis of as a genetic carrier for a specific list of qualified conditions and that the patient’s partner has a physician diagnosis of being a genetic carrier for the same condition will be provided coverage for IVF.
- Requirements/Limitations: The patient and their partner (who they intend to get pregnant with) have a physician diagnosed genetic trait associated with cystic fibrosis, spinal muscular atrophy, Morquio Syndrome, myotonic dystrophy, or sickle cell anemia.
West Virginia
-
- Coverage Mandate: HMOs must cover infertility services under the statute of those services are deemed “basic health services”. (There is no language of what infertility services must be covered or a definition of infertility).
States with IVF Exclusions or Limiting Laws
*Some states have current bills in congress to try and add coverage laws
Kansas
Medicaid insurance expressly excludes any infertility coverage
Kentucky
Medicaid insurance expressly excludes any infertility coverage
Michigan
Medicaid will cover infertility diagnosis but not treatment
Missouri
Medicaid insurance expressly excludes any infertility coverage
Nebraska
Medicaid insurance expressly excludes any fertility enhancing drugs coverage
Oklahoma
Medicaid insurance expressly excludes any infertility coverage
Oregon
Does cover basic infertility counseling for low income women, but is not a Medicaid benefit
Tennessee
Medicaid insurance specifically excludes any infertility or impotence service coverage
Wisconsin
If patients with medicaid obtain prior authorization, they insurance MAY cover certain infertility procedures
Wyoming
Medicaid insurance expressly excludes any infertility coverage
States Fertility Preservation Coverage Mandates
(which is storing eggs/sperm/embryos for later use such as cryopreservation from an IVF cycle)
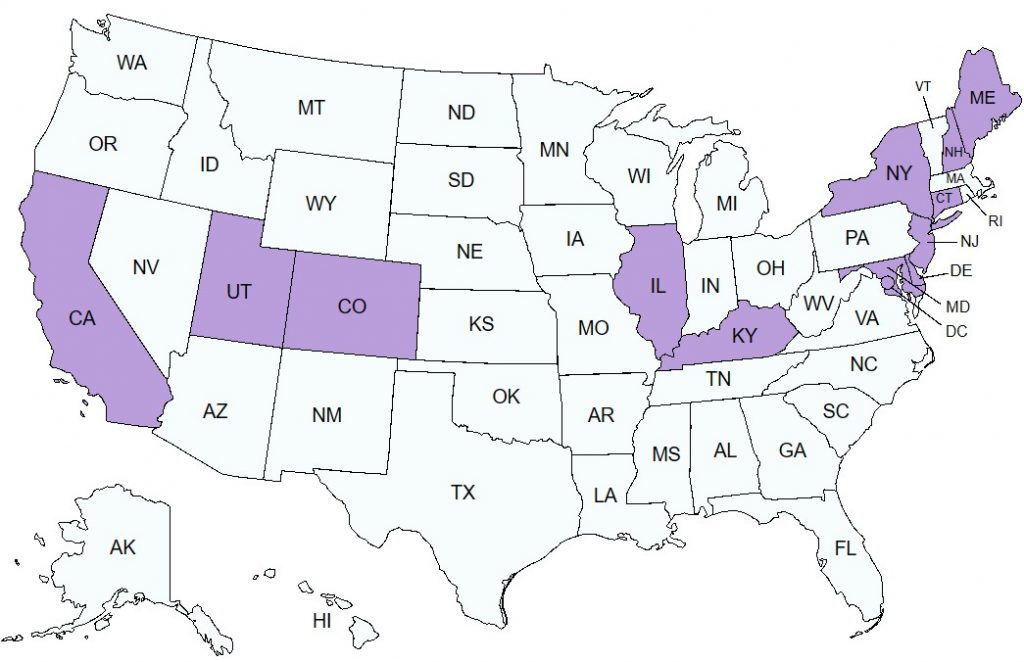
Map Key:
Purple = States with Fertility Preservation Coverage Mandates
White = States without Fertility Preservation Coverage Mandates
California
-
- Every insurance plan with basic health care services must offer standard fertility preservation services if a covered treatment may cause infertility. (Medi-Cal managed plans are exempt from fertility preservation coverage.)
Colorado
-
- Any insurance plan issued or renewed in Colorado must cover standard fertility preservation services, defined as any person who undergoes treatment that has a risk of causing infertility can undergo procedures and services deemed for fertility preservation by the guidelines from ASRM or ASCO.
Connecticut – Effective 1/1/18
- Any person that has a diagnosed medical or genetic condition that affects fertility, or who will be undergoing treatment for a medical condition that may cause infertility, is guaranteed fertility preservation services. Insurance has to cover retrieval of gametes and storage via cryopreservation until they reach 30 years of age, or 5 years after retrieval if the person is 26 or older.
District of Columbia – Effective January 1st, 2025
- All insurance plans that offer a large group, small group, or individual health plan must include standard fertility preservation services. This includes a minimum of 3 complete oocyte retrievals and unlimited embryo transfers.
Delaware
-
- Any individual who must undergo medical treatment that can cause iatrogenic fertility is guaranteed coverage for standard fertility preservation. Defines iatrogenic infertility as any medical treatment that impaired future fertility including surgery, radiation, and chemotherapy. Follows the same coverage mandate as above.
Illinois
-
- Accident and health insurance for individuals or groups must cover standard fertility preservation for patients who will undergo a medically necessary treatment that could either directly or indirectly cause iatrogenic infertility. Defines iatrogenic infertility as any medical treatment that affects reproductive organs or the reproductive process in a way that impairs fertility and includes radiation, chemotherapy, and surgery.
Kentucky (Does not have coverage mandates, but does have fertility preservation mandates) (Effective 2023)
-
- All health plans must cover fertility preservation services for both oocytes and sperm when a patient undergoes medically necessary treatment linked directly or indirectly to iatrogenic infertility. Includes any student health insurance provided by a university or college from a Kentucky-licensed insurer.
- Must cover: all expenses for evaluations, laboratory tests, medications/treatments for oocyte and sperm cryopreservation including obtaining, freezing, and we one year of storage.
- Restrictions/Limitations:
- Age limitations per ASRM and the American Society of Clinical Oncology guidelines
- Lifetime limit of one cryopreservation procedure
- Exemptions: Religious insurers do not have to cover fertility preservation
Maine (effective January 1, 2024)
-
- Any health plan in the state must cover fertility preservation services.
Maryland (Effective 10/7/2023)
-
- Maryland Medical Assistance Program will cover fertility preservation services for iatrogenic infertility defined as any medical treatments (including surgery, radiation, chemotherapy, and gender-affirming treatments) that affect the reproductive system.
- All other health care plans must cover standard fertility preservation for policyholders and covered dependents if medically necessary treatment may directly or indirectly cause iatrogenic infertility defined as impaired fertility due to surgery, chemotherapy, radiation, or medical treatment. Direct language includes cryopreservation as standard procedures, but does not include the storage of sperm or oocytes. (Religious organizations can be granted exclusion from IVF coverage and therefore may not cover standard fertility preservation procedures).
New Hampshire (Effective 1/1/2020)
-
- All health carriers must cover standard fertility preservation services for a person who will be undergoing surgery, radiation, chemotherapy, or other medical treatments that are medically recognized as a risk of causing infertility. Standard fertility preservation services including cryopreservation and storage must be covered for the duration of the policy term. Health carriers can offer optional benefits of longer storage periods.
New Jersey
-
- Under the coverage mandate, all health care services inside scope of coverage must provide standard fertility preservation services to people needing a medical treatment directly or indirectly linked to causing iatrogenic infertility.
New York (Effective 1/1/2020)
-
- Any insurance policy that provides medical care must also cover standard fertility preservation for any patient needing medical treatment which may directly or indirectly cause iatrogenic infertility. Iatrogenic infertility is defined as any medical treatment (including surgery, radiation, or chemotherapy) that can affect the reproductive organs or processes.
Rhode Island (Effective 6/16/1991)
-
- Per the coverage mandate, any insurance cover pregnancy but also cover standard fertility preservation services for any person needing medical treatment that may cause (directly or indirectly) iatrogenic infertility.
Utah (Effective 5/5/2021)
-
- Patients with Medicaid who obtain a waiver approval must be provided coverage for standard fertility preservation services. In order to gain approval, a patient must have been diagnosed with cancer by a physician and need treatment for cancer that may cause iatrogenic infertility or sterility.
